What is arthritis?
- Severe pain in one or more joints (usually not only during exercise), especially in the early morning;
- Joint pain, swelling, edema, and redness;
- The temperature of the inflammatory site increases significantly.
The inflammatory process caused by arthritis affects the entire body. In this case, the patient experiences high temperatures, chills, loss of strength, and may experience inflammation of other organs (eyes, genitourinary system, and even heart, lungs, liver, and kidneys).
- Rheumatism– Inflammation of the connective tissue of large and medium-sized joints that occurs after infection;
- Rheumatoid Arthritis– A slow autoimmune process that affects multiple joints symmetrically and simultaneously; leading to "nodules", pain, loss of mobility; can cause inflammation of many organs;
- gout– Caused by the accumulation of uric acid in the blood and salt in the joints; the most common symptom is severe pain in the big toe joint;
- reactive arthritis– Occurs against the background of damage to the body caused by infection (chlamydia, strep, etc. );
- septic arthritis– Starts due to bacterial infection of the joint itself.
What is joint disease?
- After a long period of inactivity (e. g. , a night's rest), the joints "freeze" but develop rapidly when activity resumes;
- The movement of the joints is accompanied by strange sounds (clicking, crunching, grinding);
- Physical activity can cause pain.
What is the difference between arthritis and joint disease?
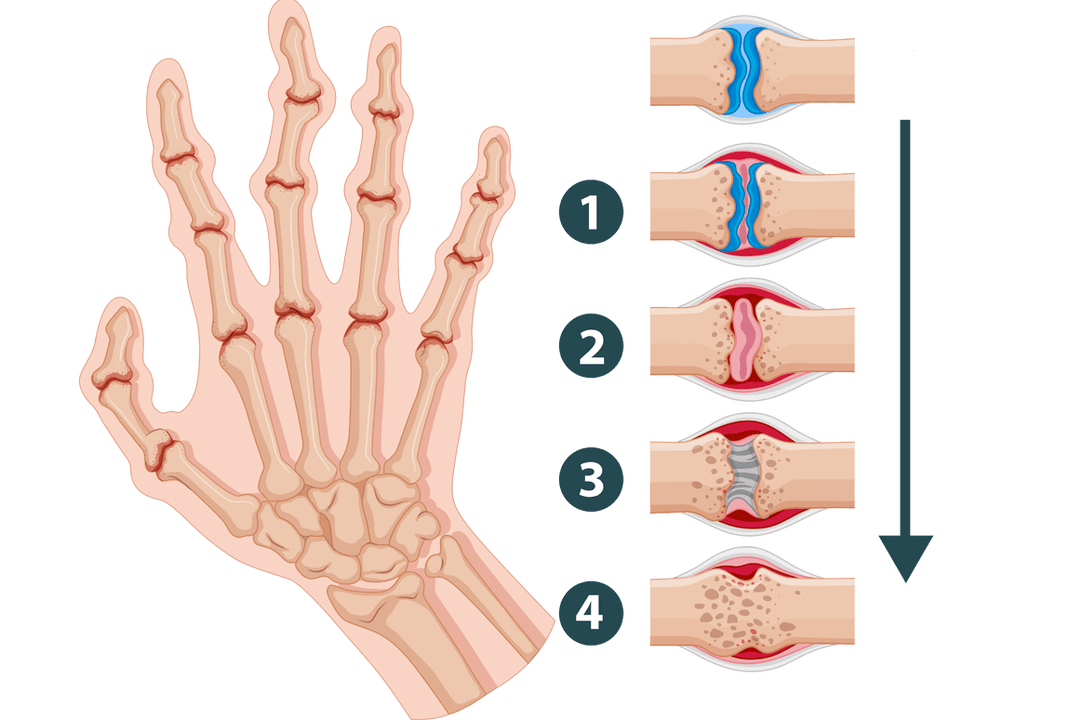
In contrast, arthritis can occur even in children. The inflammatory process leads to lesions of the synovium, which is filled with blood vessels and joint fluid (whereas arthropathy simply produces insufficient amounts). Unfortunately, almost one in five cases of disability in the world is caused by various forms of arthritis and complications.
How do arthritis and joint disease manifest?

- pain. In the initial stages of arthropathy (lasting for several years), joint pain occurs during physical activity and disappears after rest. It's rarely sharp and solid. Even as the disease progresses, pain may occur with even slight movement or even at rest, and often simply getting the body into a comfortable position is enough to relieve the pain. With arthritis, patients are plagued by severe pain that can only be relieved by special medications. A typical symptom is pain at rest, especially in the early morning.
- Clicking, grinding, or crunching sounds from the joints. In joints affected by arthrosis, the cartilage layer is destroyed. They no longer protect the heads of bones from touching each other. Therefore, as they move, the bones touch and rub against each other, making a rough, dry sound. The more advanced the disease is, the stronger and louder the clicking sound in the joints becomes. Arthritis is usually not associated with such symptoms.
- Deformation of joints and surrounding tissues. Over time, the presence of arthropathy causes changes in the shape of the bones: the heads begin to break and wear, and osteophytes may appear. Swelling and soreness sometimes occur during the acute phase, but these symptoms are not permanent. But joints affected by arthritis can become inflamed and swollen. Swelling and compaction occur. The skin becomes red and warm.
- Can not move. Osteoarthritis causes stiffness in certain joints that disappears with movement. In deeper stages, stiffness increases and flexion amplitude decreases, ultimately leading to immobility. When you have arthritis, you may feel stiffness all over your body, and trying to move causes severe pain.
- changes in blood composition. Arthropathy is not an inflammatory disease and therefore was not reflected in the analysis. Arthritis causes a significant increase in the erythrocyte sedimentation rate, which indicates active infectious and inflammatory processes.
Therefore, early joint symptoms rarely cause severe anxiety and discomfort. This can lead to a careless attitude and late diagnosis of the disease, which means further treatment becomes complicated.
Causes of Osteoarthritis
- Maintain moderate physical activity through simple exercise, walking, swimming, etc. This will help you shed excess pounds, improve blood circulation, and strengthen muscles, thereby reducing stress on your joints.
- Try to eat healthy food. Fatty foods, red meat, and alcohol can be harmful. Instead, seafood, fruits and vegetables, and dishes containing cartilage and gelatin will be beneficial. It is important to drink plenty of clean water (2-3 liters per day).
- Choose the right clothes and shoes: high heels that are comfortable, warm enough, and don’t restrict movement.
- If possible, avoid stress, distractions, and other "shocks" to the body.
For this purpose, radiography and MRI are best performed in conjunction with laboratory blood and urine tests. After studying the results, the doctor will make appropriate recommendations.
























